Surgery for “heartburn”
If you suffer from “heartburn” your surgeon, Doctor Botha, may have recommended laparoscopic anti-reflux surgery to treat this condition, technically referred to as gastro-oesophageal reflux disease (GERD). This brochure will explain to you:
- What gastro-oesophageal reflux disease (GERD) is
- Medical and surgical treatment options for GERD
- How this surgery is performed
- Expected outcomes
- What to expect if you choose to have laparoscopic anti-reflux surgery
What is gastroesophageal reflux disease (GERD)?
Although “heartburn” is often used to describe a variety of digestive problems, in medical terms, it is actually a symptom of gastroesophageal reflux disease. In this condition, stomach acids reflux or “back up” from the stomach into the esophagus. Heartburn is described as a harsh, burning sensation in the area in between your ribs or just below your neck. The feeling may radiate through the chest and into the throat and neck. Many adults in the united states experience this uncomfortable, burning sensation at least once a month. Other symptoms may also include vomiting, difficulty swallowing and chronic coughing or wheezing.
What causes GERD?
When you eat, food travels from your mouth to your stomach through a tube called the esophagus. At the lower end of the esophagus is a small ring of muscle called the lower esophageal sphincter (les). The les acts like a one-way valve, allowing food to pass through into the stomach. Normally, the les closes immediately after swallowing to prevent back-up of stomach juices, which have a high acid content, into the esophagus. GERD occurs when the les does not function properly allowing acid to flow back and burn the lower esophagus. This irritates and inflames the esophagus, causing heartburn and eventually may damage the esophagus.
What contributes to GERD?
Some people are born with a naturally weak sphincter (les). For others, however, fatty and spicy foods, certain types of medication, tight clothing, smoking, drinking alcohol, vigorous exercise or changes in body position (bending over or lying down) may cause the les to relax, causing reflux. A hiatal hernia (a common term for GERD) may be present in many patients who suffer from GERD, but may not cause symptoms of heartburn.
How is GERD treated?
GERD is generally treated in three progressive steps:
1. Life style changes
In many cases, changing diet and taking over-the-counter antacids can reduce how often and how harsh your symptoms are. Losing weight, reducing or eliminating smoking and alcohol consumption, and altering eating and sleeping patterns can also help.
2. Drug therapy
If symptoms persist after these life style changes, drug therapy may be required. Antacids neutralize stomach acids and over-the-counter medications reduce the amount of stomach acid produced. Both may be effective in relieving symptoms. Prescription drugs may be more effective in healing irritation of the esophagus and relieving symptoms. This therapy needs to be discussed with your surgeon.
3. Surgery
Patients who do not respond well to lifestyle changes or medications or those who continually require medications to control their symptoms, will have to live with their condition or may undergo a surgical procedure. Surgery is very effective in treating GERD.
There are procedures being tried, known as intraluminal endoscopic procedures, which are alternatives to laparoscopic and open surgery. You will need to discuss with your surgeon and physician whether you are a candidate for any of these procedures.
What are the advantages of the laparoscopic method?
The advantage of the laparoscopic approach is that it usually provides:
- Reduced postoperative pain
- Shorter hospital stay
- A faster return to work
- Improved cosmetic result
Are you a candidate for the laparoscopic method?
Although laparoscopic anti-reflux surgery has many benefits, it may not be appropriate for some patients. Obtain a thorough medical evaluation by a surgeon qualified in laparoscopic anti-reflux surgery in consultation with your primary care physician to find out if the technique is appropriate for you.
What to expect before laparoscopic anti-reflux surgery:
- After Doctor Botha reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an ekg depending on your age and medical condition.
- Your surgeon may request that you completely empty your colon and cleanse your intestines prior to surgery. You may be requested to drink clear liquids, only, for one or several days prior to surgery.
- It is recommended that you shower the night before or morning of the operation.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and vitamin e will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or st. John’s wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
What to expect the day of surgery:
- You usually arrive at the hospital the morning of the operation.
- A qualified medical staff member will place a small needle/catheter in your vein to dispense medication during surgery.
- Often pre-operative medications are necessary.
- You will be under general anesthesia – asleep – during the operation which may last several hours.
- Following the operation you will be sent to the recovery room until you are fully awake.
- Most patients stay in the hospital the night of surgery and may require additional days in the hospital.
How is laparoscopic anti-reflux surgery performed?
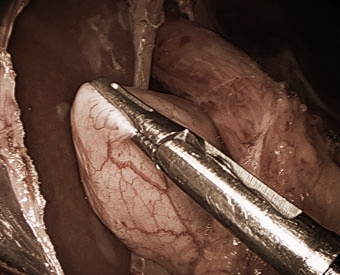
Laparoscopic anti-reflux surgery (commonly referred to as laparoscopic nissen fundoplication or toupet) involves reinforcing the “valve” between the esophagus and the stomach by wrapping the upper portion of the stomach around the lowest portion of the esophagus – much the way a bun wraps around a hot dog.
In a laparoscopic procedure, surgeons use small incisions (1/4 to 1/2 inch) to enter the abdomen through cannulas (narrow tube-like instruments). The laparoscope, which is connected to a tiny video camera, is inserted through the small incision, giving the surgeon a magnified view of the patient’s internal organs on a television screen.
The entire operation is performed “inside” after the abdomen is expanded by inflating gas into it.
What happens if the operation cannot be performed or completed by the laparoscopic method?
In a small number of patients the laparoscopic method is not feasible because of the inability to visualize or handle the organs effectively. Factors that may increase the possibility of converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, or bleeding problems during the operation. The decision to perform the open procedure is a judgment decision made by Dr Botha either before or during the actual operation. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
What should I expect after surgery?
- Patients are encouraged to engage in light activity while at home after surgery.
- Post operative pain is generally mild although some patients may require prescription pain medication.
- Anti-reflux medication is usually not required after surgery.
- Some surgeons modify patients diet after surgery beginning with liquids followed by gradual advance to solid foods. You should ask Doctor Botha about dietary restrictions immediately after the operation.
- You will probably be able to get back to your normal activities within a short amount of time. These activities include showering, driving, walking up stairs, lifting, working and engaging in sexual intercourse.
- Call and schedule a follow-up appointment within 2 weeks after your operation.
Are there side effects to this operation?
Studies have shown that the vast majority of patients who undergo the procedure are either symptom-free or have significant improvement in their GERD symptoms.
Long-term side effects to this procedure are generally uncommon.
- Some patients develop temporary difficulty swallowing immediately after the operation. This usually resolves within one to three months after surgery.
- Occasionally, patients may require a procedure to stretch the esophagus (endoscopic dilation) or rarely re-operation.
- The ability to belch and or vomit may be limited following this procedure. Some patients report stomach bloating.
- Rarely, some patients report no improvement in their symptoms.
What complications can occur?
Although the operation is considered safe, complications may occur as they may occur with any operation.
Complications may include but are not limited to:
- Adverse reaction to general anesthesia
- Bleeding
- Injury to the esophagus, spleen, stomach or internal organs
- Infection of the wound, abdomen, or blood.
- Other less common complications may also occur.
Dr Botha may wish to discuss these with you. He will also help you decide if the risks of laparoscopic anti-reflux surgery are less than non-operative management.
When to call your doctor?
Be sure to call your physician or surgeon if you develop any of the following:
- Persistent fever over 101 degrees f (39 c)
- Bleeding
- Increasing abdominal swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Chills
- Persistent cough or shortness of breath
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions that is worsening or getting bigger
- You are unable to eat or drink liquids .
More information at http://www.sages.org/